What Is Painful Heel And The Way To Fix It
Overview
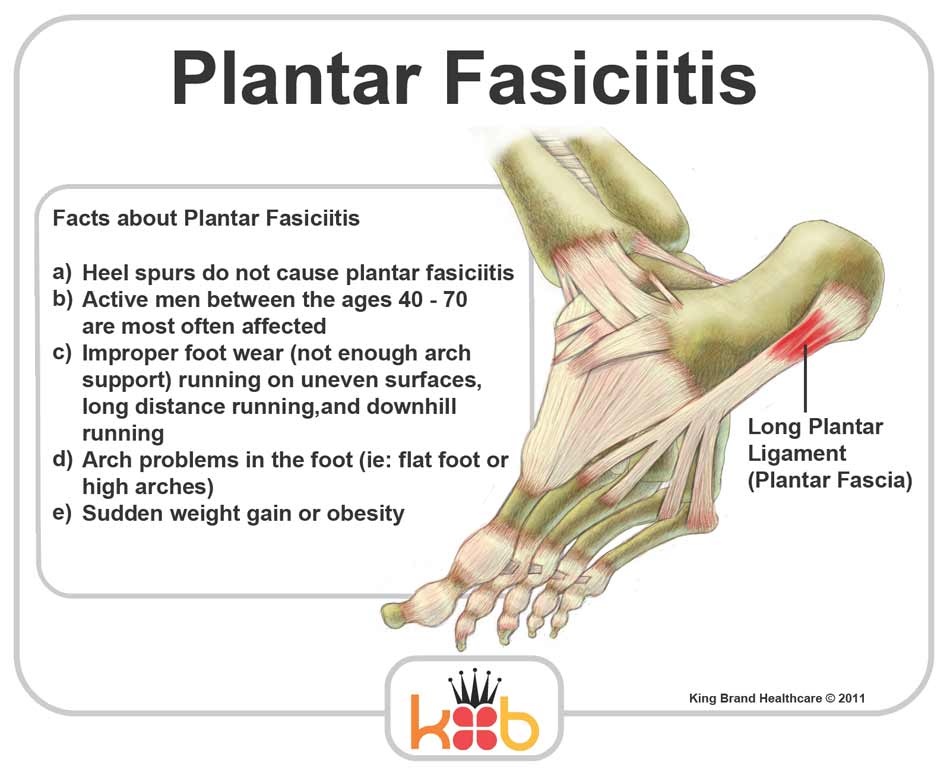
Plantar fasciitis is the most common cause of heel pain. Pain from plantar fasciitis is often most noticeable during the first few steps after getting out of bed in the morning. The plantar fascia is a thick band of tissue in the sole of the foot. Microtearing at the origin of the plantar fascia on the heel bone (calcaneus) can occur with repetitive loading. This microtearing leads to an inflammatory response (healing response) which produces the pain. Risk factors for plantar fasciitis include excessive standing, increased body weight, increasing age, a change in activity level, and a stiff calf muscle. Plantar fasciitis can be managed non-operatively in the vast majority of patients. The main components of an effective non-operative treatment program are: calf stretching with the knee straight, plantar fascia stretching, activity modification (to avoid precipitating activities), and comfort shoe wear.
Causes
There are several possible causes of plantar fasciitis, including wearing high heels, gaining weight, increased walking, standing, or stair-climbing. If you wear high-heeled shoes, including western-style boots, for long periods of time, the tough, tendonlike tissue of the bottom of your foot can become shorter. This layer of tissue is called fascia. Pain occurs when you stretch fascia that has shortened. This painful stretching might happen, for example, when you walk barefoot after getting out of bed in the morning. If you gain weight, you might be more likely to have plantar fasciitis, especially if you walk a lot or stand in shoes with poor heel cushioning. Normally there is a pad of fatty tissue under your heel bone. Weight gain might break down this fat pad and cause heel pain. Runners may get plantar fasciitis when they change their workout and increase their mileage or frequency of workouts. It can also occur with a change in exercise surface or terrain, or if your shoes are worn out and don't provide enough cushion for your heels. If the arches of your foot are abnormally high or low, you are more likely to develop plantar fasciitis than if your arches are normal.
Symptoms
Pain tends to start gradually, often just in the heel, but it can sometimes be felt along the whole of the plantar fascia. The symptoms are initially worse in the morning and mostly after, rather than during, activity. As the condition becomes worse, the symptoms become more persistent.
Diagnosis
After you describe your symptoms and discuss your concerns, your doctor will examine your foot. Your doctor will look for these signs. A high arch, an area of maximum tenderness on the bottom of your foot, just in front of your heel bone. Pain that gets worse when you flex your foot and the doctor pushes on the plantar fascia. The pain improves when you point your toes down. Limited "up" motion of your ankle. Your doctor may order imaging tests to help make sure your heel pain is caused by plantar fasciitis and not another problem. X-rays provide clear images of bones. They are useful in ruling out other causes of heel pain, such as fractures or arthritis. Heel spurs can be seen on an x-ray. Other imaging tests, such as magnetic resonance imaging (MRI) and ultrasound, are not routinely used to diagnose plantar fasciitis. They are rarely ordered. An MRI scan may be used if the heel pain is not relieved by initial treatment methods.
Non Surgical Treatment
Treatment for heel pain usually involves using a combination of techniques, such as stretches and painkillers, to relieve pain and speed up recovery. Most cases of heel pain get better within 12 months. Surgery may be recommended as a last resort if your symptoms don't improve after this time. Only 1 in 20 people with heel pain will need surgery. Whenever possible, rest the affected foot by not walking long distances and standing for long periods. However, you should regularly stretch your feet and calves using exercises such as those described below. Pain relief. Non-steroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, can be used to help relieve pain. Some people also find applying an ice pack to the affected heel for 5-10 minutes can help relieve pain and inflammation. However, do not apply an ice pack directly to your skin. Instead, wrap it in a towel. If you do not have an ice pack, you can use a packet of frozen vegetables.

Surgical Treatment
Surgery is considered only after 12 months of aggressive nonsurgical treatment. Gastrocnemius recession. This is a surgical lengthening of the calf (gastrocnemius) muscles. Because tight calf muscles place increased stress on the plantar fascia, this procedure is useful for patients who still have difficulty flexing their feet, despite a year of calf stretches. In gastrocnemius recession, one of the two muscles that make up the calf is lengthened to increase the motion of the ankle. The procedure can be performed with a traditional, open incision or with a smaller incision and an endoscope, an instrument that contains a small camera. Your doctor will discuss the procedure that best meets your needs. Complication rates for gastrocnemius recession are low, but can include nerve damage. Plantar fascia release. If you have a normal range of ankle motion and continued heel pain, your doctor may recommend a partial release procedure. During surgery, the plantar fascia ligament is partially cut to relieve tension in the tissue. If you have a large bone spur, it will be removed, as well. Although the surgery can be performed endoscopically, it is more difficult than with an open incision. In addition, endoscopy has a higher risk of nerve damage.